Recently, the Digestive Department team of Zhejiang Chinese Medical University, in collaboration with Changxing County People's Hospital, published a special article titled 'Constipation is Not Scary; Correct Medication is Key' in the national medical journal Physician Online. The article systematically reviews the pathological mechanisms, health risks, prevention and treatment strategies of constipation, as well as the mechanisms of action and clinical application effects of plecanatide. Through this authoritative medical platform, the paper conveys knowledge about intestinal health and the concept of scientific medication to the public, attracting widespread attention.
According to WHO data, more than 1 billion people worldwide suffer from diarrhea or constipation, with 400,000 new colorectal cancer cases each year. In China, there are 17 million people with constipation (accounting for 1.21%), and the prevalence of chronic constipation in adults is 4%-6%, reaching 22% in those over 60, with a recurrence rate of 40%. Constipation is related to factors such as diet, prolonged sitting, and medications, with pregnant women and postoperative patients considered high-risk groups. Long-term constipation can lead to cardiovascular and cerebrovascular diseases as well as intestinal disorders, but public awareness is insufficient, and the misuse of laxatives is common. Scientific prevention and treatment should start with adjusting lifestyle habits, and bulk-forming laxatives like Lipofer® Polycarbophil Calcium can soften stool by absorbing water, gently improve bowel movements, avoid stimulant dependence, and help build a barrier for gut health management.
1. Pathological Analysis of Constipation
Constipation is the result of the combined effects of abnormal intestinal motility and dysregulation of the defecation reflex. Its pathological mechanisms can be summarized into three core components:
(1). Intestinal motility disorders: Reduced contraction of the intestinal smooth muscle or dysfunction of the enteric nerves leads to delayed colonic transit, commonly seen in the elderly, diabetic patients,and sedentary individuals. A lack of dietary fiber or excessive water absorption in the colon can exacerbate the hardening of intestinal contents, forming a vicious cycle.
(2). Dysregulation of the defecation reflex: An elevated rectal sensory threshold or coordination disorder of the pelvic floor muscles (such as puborectalis spasm) causes difficulty in defecation. This often occurs secondary to anorectal conditions (hemorrhoids/anal fissures), metabolic diseases (uremia/hypothyroidism), or neurological disorders (Parkinson's disease/spinal cord injury).
(3). Neuropsychiatric and drug-related factors: Anxiety and depression can activate the sympathetic nervous system to inhibit intestinal peristalsis. Certain antidepressants, calcium channel blockers, and chemotherapeutic drugs (such as vinca alkaloids) can directly damage the enteric autonomic nerves through neurotoxicity, inducing colonic motility disorders. The interaction of these multiple factors results in constipation being recurrent and difficult to treat, necessitating comprehensive interventions targeting the underlying pathological mechanisms.
2. Health Risks of Constipation
(1). Organic damage to the intestines: Long-term difficulty in defecation leads to repeated sudden increases in intra-abdominal pressure, causing congestion and expansion of the anal venous plexus and forming hemorrhoids; persistent friction of hard stool against the rectal mucosa can result in erosion, ulcers, or even proctitis, with severe cases showing bloody discharge. Colonic motility disorders cause fecal retention, leading to cecal dilatation and megacolon, resulting in irreversible atrophy of the intestinal muscular layer.
(2). Microbiota-inflammatory-neural damage: Imbalance in the gut microenvironment triggers overgrowth of pathogenic bacteria (such as Escherichia coli), releasing lipopolysaccharides that activate immune responses. Persistent elevation of pro-inflammatory factors (TNF-α) leads to chronic low-grade inflammation. This 'leaky gut' condition damages the enteric nervous system, accelerates neuronal apoptosis, creates a vicious cycle of delayed colonic transit, and increases the risk of adenomatous polyps.
(3). Systemic metabolic and immune disorders: Dysbiosis promotes metabolic endotoxemia via the gut-liver axis, inducing insulin resistance and visceral fat accumulation, exacerbating metabolic syndrome. Straining during defecation causes sudden blood pressure spikes (up to 200/110 mmHg), significantly raising the risk of acute cardiovascular events. In addition, reduced secretion of intestinal secretory immunoglobulin A (sIgA) leads to increased susceptibility to respiratory infections and delayed wound healing.
(4). Neuropsychiatric damage: Disturbances in the gut-brain axis transmit abnormal signals via the vagus nerve, causing anxiety, depression, and other emotional disorders. Reduced microbial metabolites (such as short-chain fatty acids) hinder the synthesis of brain-derived neurotrophic factor (BDNF), with hippocampal atrophy in elderly patients manifesting as cognitive decline. This systemic damage mechanism makes constipation an important early-warning indicator reflecting overall health.
3. Methods for Preventing and Treating Constipation
(1). Daily Prevention of Constipation
To prevent and treat constipation, it is important to maintain a healthy daily diet, engage in moderate exercise, and develop a regular bowel habit. It is recommended to consume at least 25-30g of dietary fiber and more than 1.5L of water daily. Drinking warm water or lightly salted water on an empty stomach in the morning is beneficial. Ensure about 150 minutes per week of activities such as brisk walking or yoga, and combine with clockwise abdominal massage for 10 minutes. Develop a regular bowel routine and do not suppress the urge to defecate.
(2). Medication Treatment for Constipation
2.1 Pharmacological Action of Libope® Polycarbophil Calciu

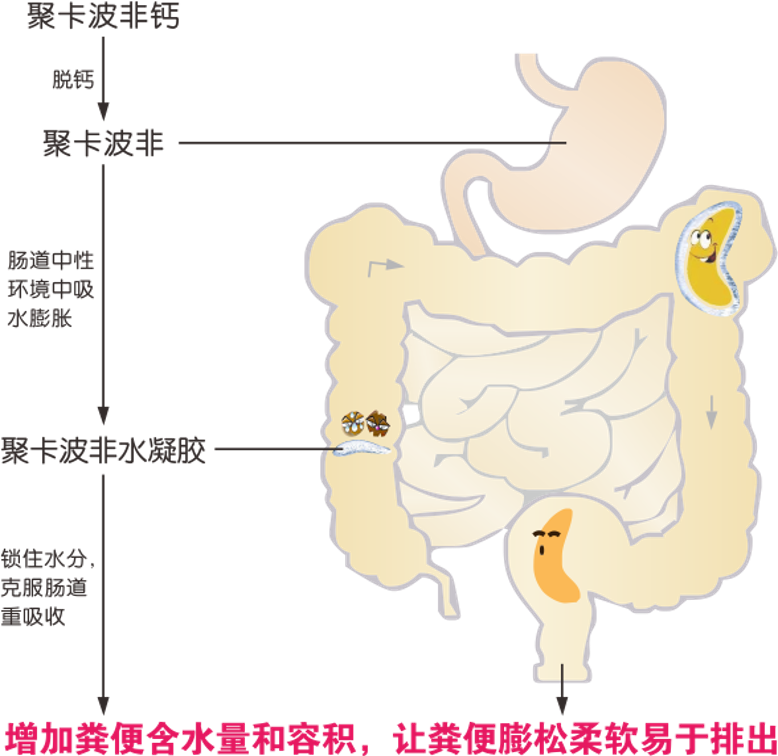
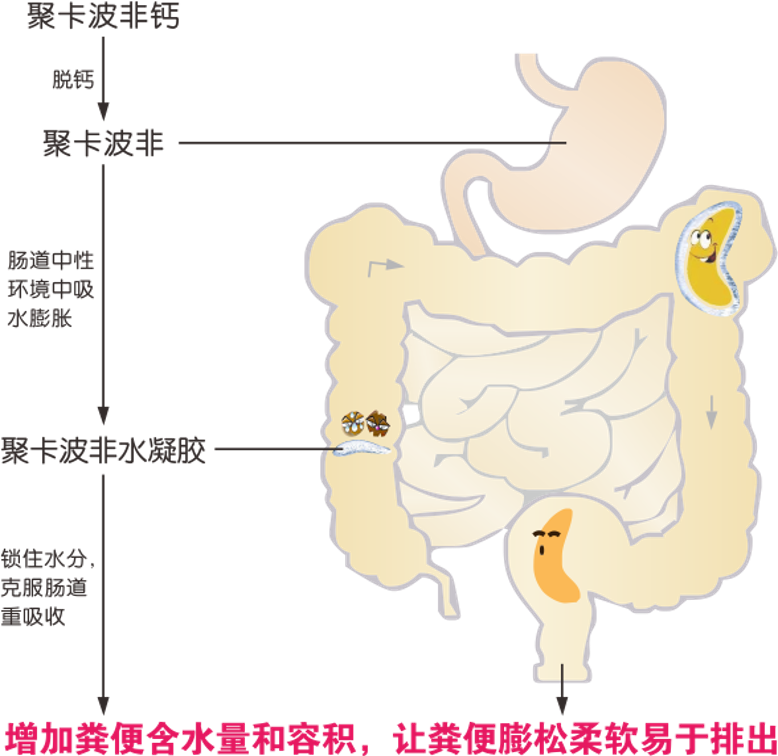
When the above interventions are ineffective, medication should be used appropriately under the guidance of a doctor. Lipofe® Polycarbophil Calcium, as a bulk-forming laxative, triggers a decalcification reaction in the acidic environment of the stomach to release polycarbophil. Once it enters the intestines, it absorbs water and expands to form a gel matrix, increasing stool volume to mechanically stimulate bowel movements while also absorbing excess water to prevent dry stools, thereby reducing intestinal burden. Its physical mechanism of action avoids the risk of drug dependence and intestinal nerve damage, making it especially suitable for pregnant women, the elderly, children, and patients with chronic constipation who require long-term medication. The mechanism of action is shown in Figure 2.
2.2 Usage and Clinical Efficacy of Lipofef® Polycabof Calcium
Follow the doctor's instructions and take with a sufficient amount of water after meals. Numerous clinical trials have shown that the proper and reasonable use of Lipofen® Polycarbophil Calcium in treating constipation is not only effective but also safe and reliable.
For example, clinical experiments on mice and dogs have shown that as the administration time increases, the cumulative fecal excretion rate of mice and dogs significantly increases during the first 2–3 days, then stabilizes, maintaining a range of 96.3% ± 2.0 and 101.6% ± 1.7, respectively.
A domestic randomized, double-blind, multicenter, placebo-controlled trial of polycarbophil calcium in the treatment of IBS-C (constipation-predominant irritable bowel syndrome) found that using polycarbophil calcium 1 g, tid, for 4 consecutive weeks effectively improved the overall symptoms of constipated patients (average overall symptom improvement after four weeks was 0.935, much higher than 0.59 in the placebo group).
In a study of 192 patients with fecal incontinence taking polycarbophil calcium 1.5–3.0 g/day as monotherapy for one month, 14% of patients fully recovered, and 71% showed significant improvement. The number of patients with a Bristol score of 3–4 increased from 55 before treatment to 111 after treatment, indicating that polycarbophil calcium significantly improves fecal incontinence and stool consistency in patients.
In summary, constipation is a common and prevalent gastrointestinal condition that can pose multiple harms and impacts on human health. However, constipation is not to be feared; with the right methods and medications, it can be both preventable and treatable.
References[1] Yang Hui. Constipation is not frightening; correct medication is key [J]. Physician Online, 2025, 10. DOI:6jrvyke7pd/9215087.

Scan to view the original text
 Fulexin® Cefuroxime Axetil Tablets
Fulexin® Cefuroxime Axetil Tablets Keluo® Cefaclor Capsules
Keluo® Cefaclor Capsules Kefu® Cefaclor Granules
Kefu® Cefaclor Granules Mieda® Cefradine Capsules
Mieda® Cefradine Capsules Lvxin® Cefalexin Capsules
Lvxin® Cefalexin Capsules Lifu® Roxithromycin Capsules
Lifu® Roxithromycin Capsules Lifu® Roxithromycin Granules
Lifu® Roxithromycin Granules Tinijin® Tinidazole Capsules
Tinijin® Tinidazole Capsules Fulexin® Cefazolin Sodium for Injection
Fulexin® Cefazolin Sodium for Injection Wolexin® Cefepime Hydrochloride for Injection
Wolexin® Cefepime Hydrochloride for Injection Xiulexin® Ceftizoxime Sodium for Injection
Xiulexin® Ceftizoxime Sodium for Injection Xinlexin® Ceftriaxone Sodium for Injection
Xinlexin® Ceftriaxone Sodium for Injection Weilexin® Cefonicid Sodium for Injection
Weilexin® Cefonicid Sodium for Injection Yuelexin® Cefoxitin Sodium for Injection
Yuelexin® Cefoxitin Sodium for Injection Lilexin® Cefodizime Sodium for Injection
Lilexin® Cefodizime Sodium for Injection Ailexin® Cefpirome Sulfate for Injection
Ailexin® Cefpirome Sulfate for Injection